Why Gay Intended Fathers Should Care More About Their Sperm
I hate to admit it - again - but RFK Jr. was right. We do have a sperm problem. And by we, I mean modern day men in the developed world. Data shows that we have lower testosterone and sperm than previous generations.
As a gay man having children through IVF and surrogacy, I honestly didn’t think my sperm health mattered all that much. I mean, it’s not like we’re conceiving naturally where the number and motility of the sperm play a vital role. The reproductive endocrinologist just needs a handful of sperm to fertilize the eggs through intracytoplasmic sperm injection (ICSI).
So, why should gay men who want to have children through assisted reproduction care about their sperm? In this article, I hope to provide some fertility and financial reasons why the health of your sperm does matter for your rainbow family building.
IVF for Gay Men
In addition to a brief physical exam and some blood testing, the medical screening for gay intended dads rests heavily on the sperm donation. You can read all about my experience leaving my deposit in the clinic in LA.
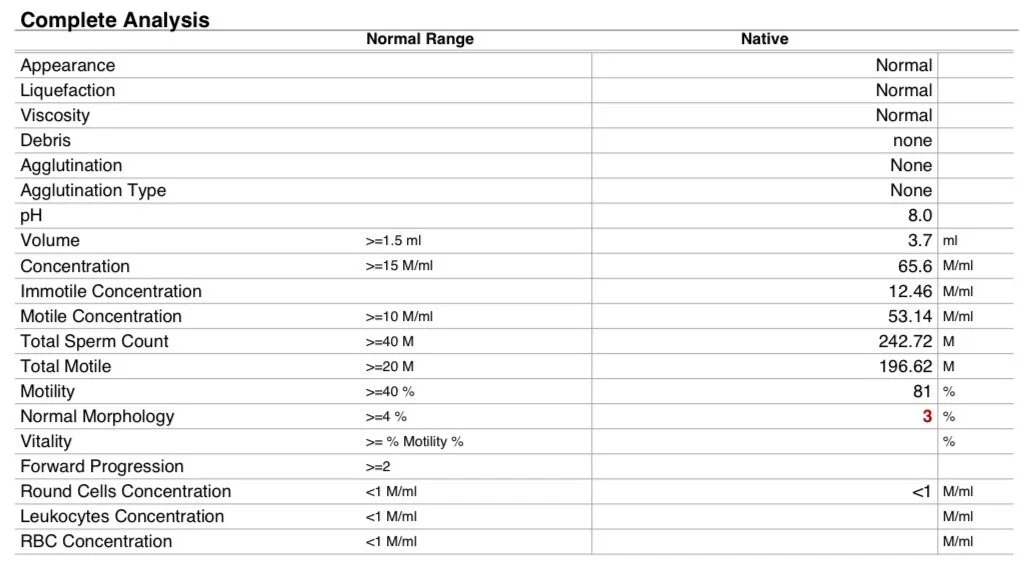
Our sperm results came back average in most areas, while mine was slightly below the threshold for the percentage of sperm having normal morphology (or shape).
My sperm sample results
No matter, it’s not like my sperm were going to swim or make their way into the egg themselves. They were just going to be injected in, so their shape shouldn’t matter…right?
Most of the scrutiny for gametes in IVF comes to the egg. Much attention was focused on the egg donor’s age, her anti-mullerian hormone (AMH), evidence from previous retrievals, and her overall medical and family history.
It feels like all the pressure to perform for the embryo is on the egg.
After our egg retrieval, both my husband and my sperm were thawed and ICSI was used to fertilize half the eggs with each sperm.
Our ‘Embryonic Olympics’ as I called them, resulted in 3 PGT embryos that we now have waiting for transfer.
This is great. We are thrilled to have these three embryonic champions. But I thought, is there anything we could have done to have more?
You Don’t Have to Do ICSI
I’m a physician, and I never thought to question ICSI. However, I realized only after our embryo creation that there is another way.
Yes, ICSI is recommended when using thawed sperm, but what if the deposit was fresh?
You could pursue an option called conventional IVF (c-IVF). In c-IVF, an egg is surrounded by sperm in a Petri dish and ultimately one sperm fertilizes the egg. It’s a more ‘natural’ process where the sperm compete for the egg.
The challenges with c-IVF are all around timing. Research has been done to analyze ideal time ranges for after the egg retrieval (studies show between 3 and 6 hours after egg retrieval are optimal), time the sperm and egg are together in the Petri dish (overnight is standard, but shorter times do not show significant differences in live birth rates), and factors such as oxygenation (which still requires further research) (1).
While there is no question that ICSI is preferred when there are severe sperm issues, there is less evidence that it is needed or even better than c-IVF when there is no male factor infertility, such is the case with my husband and me.
A recent study in Nature sought to compare the efficacy of c-IVF and ICSI (2). The researchers conducted a large, randomized clinical trial involving 824 women undergoing their first IVF cycle. They were randomized to ICSI (n = 414) or c-IVF (n = 410) across six public fertility clinics in Denmark. The results compared the ideal endpoint of live birth rates and found there was no difference between the groups. The live birth rate was 43.2% (179/414) in the ICSI group and 47.3% (193/408) in the c-IVF group. Their conclusions were that there was no benefit to ICSI for male patients with normal or nonseverely decreased sperm quality, and they stated that ICSI should be reserved for severe male factor infertility.
ICSI is More Expensive
While c-IVF does pose some logistical challenges in terms of coordinating egg retrievals and sperm deposits, which can be especially hard for international IPs like my husband and I, it does allow for a more natural selection process. This may seem counterintuitive in IVF, but I do find there to be something interesting about having the sperm decide who fertilizes the egg as opposed to the lab. Just with Darwinian natural selection in the wild, the most fit sperm is most likely to fertilize the egg, and so the overall health of sperm is critical for success in c-IVF.
Unsurprisingly, having the fertility lab choose the fittest sperm also adds additional costs to the process.
A 2024 article found that ICSI costs an additional $1,500 when compared with c-IVF (3). Utilizing the CDC Fertility Database that I have previously analyzed, the authors found that over a 2 year period, clinics across the U.S. were charging an additional $7,386,980 to $7,562,180 to patients for the use of ICSI routinely.
While $1,500 does not seem like a lot when the price tag of a U.S. surrogacy journey is over $200,000, I think all intended gay dads will agree with me when I say that every little savings matters in this journey.
Okay, But I Still Want to Do ICSI
Whether it’s for the cost savings related to the travel, convenience of freezing your sperm, or because your fertility clinic recommends ICSI for all cycles, it’s still a good option.
However, the health of your sperm still matters.
Studies have shown that sperm quality has an effect on embryo development even with ICSI (4). Fertilization and cleavage rates, quality of embryos as well as blastocyst development rates were significantly reduced as semen concentration, motility, and morphology decreased.
So, it’s possible that my slightly below normal morphology affected the number and quality of our embryos.
It’s important to note that fertility labs are not selecting sperm at random. They have techniques for selecting sperm for ICSI, with some of these processes mimicking natural conception (5). However, there are about a dozen different methods, and there is still debate as to what the ‘gold standard’ techniques are (6).
AI has recently been incorporated into this process. Researchers at Columbia University have developed the STAR system, where cutting-edge AI, high-speed imaging, and robotics can detect and retrieve even the smallest number of sperm gently (7). While this is initially targeted at men with little to almost no sperm, I am sure such technology could further be developed to detect additional characteristics for selecting the most optimal sperm for any ICSI procedure.
In the future, artificial selection of sperm through ICSI may lead to more live births than through natural selection through c-IVF, but it doesn’t seem like this is currently the case.
Either way, your sperm health matters for the number and quality of your embryos.
I Get It. My Sperm Health Matters as a Gay Intended Dad. So What Do I Do?
Great question. In the next BabyMoon Family article, I am going to review all the lifestyle and medical changes that queer intended dads can make in order to make their sperm fit as a fiddle for its time in the IVF lab.
References: